The human excretory system plays a crucial role in maintaining the body’s internal balance by removing waste products and toxins. It consists of organs like the kidneys, ureters, bladder, and urethra, which work together to filter blood, regulate water levels, and expel harmful substances through urine. This system ensures that metabolic waste, such as urea and excess salts, does not accumulate in the body, preventing toxicity and maintaining overall health. Understanding the human excretory system helps us appreciate its significance in homeostasis and the efficient functioning of other body systems.
Components of the Human Excretory System
- A pair of kidneys
- A pair of ureter
- One urinary bladder
- Urethra
Human kindneys are retroperitoneal meaning unlike the gut, the peritoneal membrane does not completely surround the kidney rather only half of the kidney is ventrally covered by the peritoneal membrane. This is called retroperitoneal condition.
Human kidney including mammals has METANEPHRIC KIDNEY. In other words, during the embryonic stage, only the posterior part of the kidney develops into functional kidney.
| Size of kidney | Weight of kidney |
| 10-12 cm length, 5-7 cm width, 2-3 cm thickness
|
120-170 gram
|
Types of Kidney

PRONEPHROUS KIDNEY:
- Uriniferous tubules are segmentally arranged
- Glomerulus absent
- Nephrostome present and functional
- Commonly called Head Kidney (present in anterior side of the body)
- Kidney is not differentiated into cortex and medulla
- The duct arising from kidney is called PRONEPHRIC DUCT
- PCT, Henle’s loop and DCT are not differentiated
- Example: Adults: Myxine (Hag fish); Embryos – fishes and amphibians (tadpole larva of frog)
MESONEPHRIC KIDNEY:
- Nephrons are not segmentally arranged
- Glomerulus internal
- Nephrostome – present / absent, if present – non-functional
- Commonly called Middle Kidney
- Not differentiated into cortex and medulla
- Duct of the kidney is called Mesonephric duct or Wolffian duct
- PCT, Henle’s loop and DCT are not differentiated
- Adults – fishes and amphibians. Embryos: reptiles, birds, and mammals
METANEPHRIC KIDNEY
- Nephrons are not segmentally arranged
- Glomerulus internal
- Nephrostome absent
- It is a posterior kidney
- It is differentiated into cortex and medulla
- Duct of such kidney is called metanephric duct or ureter
- PCT, Henle’s loop and DCT are very well differentiated
- Adults: reptiles, birds, and mammals; not present in embryonic stages
Location of Kidney of the Human Excretory System
The location of kidney is from T12 to L3

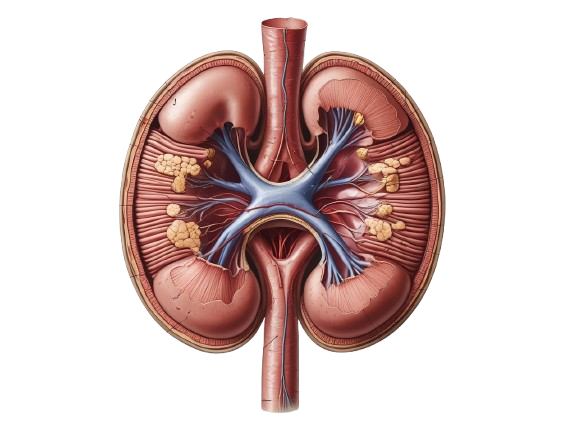
L.S of Kidney of the Human Excretory System

STRUCTURE OF THE URINARY SYSTEM

Ureters are hollow tube. Innermost wall is made up of transitional epithelium, which has the property of stretching. Middle layer is muscular (both longitudinal and circular muscles). The outermost layer is connective tissue sheath (tunica adventitia). In the ureter, urine moves through peristalsis.
Urinary bladder: its histology is similar to the ureter, only its muscular layer is called detrusor muscle (consisting of three layers of muscles: longitudinal – outermost; circular – middle; longitudinal — innermost). There is a cone structure inside the urinary bladder, called trigone. In this trigone, two urinary duct opens and one urethra. The capacity of the urinary bladder is 700 – 800 ml. However, when the urinary bladder is filled with up to 500 ml urine – a person feels the urge to urinate. Micturition is the process of passing out (voiding) the urine. Incontinence is a condition where the bladder fills and leaking of urine starts due to the defect in controlling the sphincter.

STRUCTURE OF NEPHRON of THE HUMAN EXCRETORY SYSTEM
In each kidney about 1-1.2 million nephrons are present.
Nephron / uriniferous tubule is the functional unit of the kidneys. Nephron comprises of two parts:
- Renal tubule
- Glomerulus

Nephron will consist of Bowman’s capsule, PCT, Loop of Henle, DCT (CT will not be considered as a part of the neprhron).
HISTOLOGY OF THE NEPHRON
Bowman’s capsule: Glomerular capillaries + two layers of epithelial cells + Mesangial cells
- Outer lining of the capsule is simple squamous epithelium
- Inner lining of capsule is also made of simple squamous epithelium, called PODOCYTES (fine finger like projections arise from the podocyte cell)
Note: the inner podocytes are embedded on the glomerular capillaries. However, the outer Bowman’s capsule layer is surrounding the inner podocyte layer. And in between the outer and inner lining, a gap is present. In other words, Bowman’s capsule is nothing but a two layered cells wherein a gap is present between the two layers of cells, called Bowman’s space. The Bowman’s capsule is not circular rather it is open on both sides. However, it connects to proximal cells to form the PCT.

The space between capillaries are filled by up by mesangial cells and matrix. The visceral endothelial cells are lined by the basement membrane. And the inner capillary wall is lined by specialized endothelial cells with holes (70-90 nm) within the cell. And capillaries bearing these specialized endothelial cells are called FENESTRATED CAPILLARIES. However, there is no visible pore present in the basement membrane (which could be about 8nm). In other words, we can say that the effective filtration through the filtration membrane is due to the presence of the basement membrane. Smallest blood protein is albumin which is 7-8 nm cannot pass through the filtration membrane. So, particles smaller in size than albumin can only pass through the filtration membrane.
BOWMAN’S CAPSULE + GLOMERULUS = RENAL CAPSULE / MALPHIGIAL CORPUSCLE

PCT: Proximal Convoluted Tubule
- It is lined by brush bordered cuboidal epithelium. Brush bordered means these cell membranes have lot of microvilli and their cytoplasm consists of lots of mitochondria as they are involved in active transport. The glomerular filtrate which is isosmotic to blood plasma enters the PCT where the filtrate volume is reduced by about 80%. This reduction in filtrate volume is accomplished by the active reabsorption of NaCl, glucose, amino acids, etc from the tubular fluid. As these solutes are removed, the tubular fluid becomes hyposmotic and the interstitial fluid surrounding the tubular wall becomes hyperosmotic. This causes passive diffusion of water out of the renal tubule to restore isosmotic condition between the tubular fluid and the surrounding cortical interstitium. This reabsorption of water is secondary to solute transport and occurs inevitably irrespective of the water requirements of the body. Hence it is called obligatory reabsorption of water. Thus. in PCT, there is a drastic reduction in fluid volume withour any change in its osmolarity.

Loop of Henle
Thick segment is having simple cuboidal epithelium
Thin segment is having simple squamous epithelium
The descending Loop of Henle is permeable to water only. Water moves out of the renal tubule and the filtrate becomes more concentrated as we move down the descending limb.
Ascending Loop of Henle: the tubular fluid from the descending Loop of Henle passes through the hair-pin bend of the loop, and enters the ascending limb of Henle’s loop. The walls of ascending loop do not permit diffusion of water, but salts only.
DCT: Distal Convoluted Tubule
- Its structure is similar to PCT, but has less mitochondria, and microvilli. The hyposmotc fluid from the ascending Loop of Henle enters the DCT. Under conditions of water diuresis i.e., when there is no need for water conservation, the hyposmotic tubular fluid passes into the CT unchanged in its osmolarity. However, when the water is to be conserved by the body, the ADH which makes the wall of the DCT permeable to water. So, when the ADH level is high in the blood, water difuses out of the DCT and fluid becomes isosmotic to blood by the time it enters the CT.
CT: Collecting Duct
- It is lined by simple cuboidal epithelium. The fluid that reaches the CT may be hyposmotic or isosmotic depending on the water status of the animal. Final adjustments in urine compositon are made in the CT whose walls are permeable only in the presence of ADH. In the absence of ADH, as it happens during dieresis, the hyposmotic fluid that enters the CT passes through the latter unchanged.
Nephrons can be classified into two categories:

Cortical nephron (major nephron):
- 85 % of the total nephron, shorter in length. It works like forming urine under normal condition where there in so scarcity of body fluid; vasa recta (a minute peritubular blood vessles runs parallel to the Henle’s loop forming a U shaped vasa recta) are absent. The loop of Henle is too short and extends only very little into the medulla.
Juxtamedullary nephron:
here the nephron starts at the junction of the cortex and the medullary region. They are less in number (15%); longer in length; vasa recta present. It works like form urine under water stress condition. It has long loop of Henle and runs deep into the medulla.
JUXTAGLOMERULAR APPARATUS (JGA): it is formed by the combined structure of the glomerulus and distal convoluted tubule cells.

The part of the DCT falling near to the glomerular capillaries consists of columnar cells forming a dense structure, called macula densa. On the afferent arteriole some muscle cells (myocytes) are modified to form Juxtaglomerular (JG) cells. Some cells are present between the macula densa and glomerular capillaries, called Laci’s cells, but their functions are not known yet.
JGA = JG cells + Macula densa + Laci’s cells
JG cells are endocrine in nature and secrete a hormone, called RENIN only when they get a message from the macula densa. The macula densa acts like a sensor. The filtrate passing through the DCT is observed by the macula densa – if water, Na and Cl are low in the DCT, then macula densa will get activated and that will send a message to the JG cells so as to release RENIN. And thus the Na could be reabsorbed.
OSMOREGULATION MECHANISM OF THE HUMAN EXCRETORY SYSTEM
(A) RAAS (Renin Angiotensin Aldosterone System): this is activated when blood volume is low or low blood pressure (low Na, Cl).
- What are the organs involved in RAAS activation?
- Following are the organs involved in RAAS activation:
- Circulatory system
- CNS
- Kidney
- Liver
- Pulmonary circulatory system
- Adrenal cortex
ANALOGY
Suppose a person met an accident and bleeding profusely. His blood pressure and blood volume is going down. This will also decrease the blood flow to the kidney i.e., to the afferent arteriole. This triggers kidney to produce more renin and send it to the circulatory blood. First of all we need to understand how kidney produces renin under low blood pressure. When blood with low pressure passes through the afferent arteriole, a blood pressure measuring device (baroreceptor) called JG cells (specialized smooth muscles) present on the afferent arteriole get activated and release RENIN into the blood through the efferent arteriole. On the other hand, some specialized cells are present at the junction of the ascending loop of Henle and the DCT, called MACULA DENSA – these cells are Na measuring device (Chemoreceptor).
In normal GFR (120 ml/min), 65% of Na is absorbed in PCT and 25 % Na in the ascending loop of Henle, It means, only 10 % of Na reaches the DCT. In case of low blood pressure, the GFR rate will decrease and the filtrate will move through the renal tubule slowly. As a result the renal tubular cells get enough time to absorb extra amount of Na. And by the time, the fluid reaches the DCT, it will have less than 10% Na. And when there is less Na in the DCT, the macula densa gets activated; it releases prostaglandins to activate the JG cells to release more and more RENIN. The function of RENIN is to bring the blood pressure and blood volume up.
When a person bleeds profusely, the carotid sinus (another blood pressure measuring device) of the heart receives less blood and thus sends a signal to the CNS that the blood pressure is falling. The sympathetic neurons will connect to the JG apparatus and release norepinephrin. Thus results in more release of RENIN to the blood. The hormone RENIN will go to the general blood circulation or systemic blood circulation. Now, we focus on the liver. This is the organ that produces different types of proteins including ANGIOTENSINOGEN (a plasma protein) all the time during normal blood circulation in an inactive state. It means, we can find ANGIOTENSINOGEN in the blood all the time. As soon as RENIN comes into the blood, it works on ANGIOTENSINOGEN and converts it into ANGIOTENSIN I. Now, when ANGIOTENSIN I passes through the pulmonary circulation, it changes into ANGIOTENSIN II, it means, there must be an enzyme present in the lungs responsible for converting ANGIOTENSIN I into ANGIOTENSIN II. That enzyme is called ANGIOTENSIN CONVERTING ENZYME (ACE). Now the question is what ANGIOTENSIN II will do in our body? It will surely increase the blood pressure and blood volume in the body. First of all, ANGIOTENSIN II acts as a VASOCONSTRICTOR. There are receptors present on areterial and venus smooth muscles. So, when ANGIOTENSIN II binds with the receptor, say the venus smooth muscles, it causes constriction in the blood vessel as a result, more blood will be sent to the heart. (70% of the total human blood is accumulated in the vein).
On the other hand, when ANGIOTENSIN II reaches the arterial smooth muscle receptor, it increases the cardiac output and finally increases systolic blood pressure. There is another receptor for ANGIOTNSIN II which is present on adrenal cortex (ZONA GLOMERULOSA). When these receptors are activated, the cells of the ZONA GLOMERULOSA start releasing ALDOSTERONE. Through the blood circulation, aldosterone will reach to the P cell (specialized cell present between DCT AND CT). The activated cell produces protein that reaches to the vasolateral membrane of the cell except luminal membrane. These proteins are nothing but Na-K ATPase. Under the influence of ALDOSTERONE, the cell starts throwing Na ions into the extracellular fluid and getting in the K ions. As a result, such cells become extremely poor in Na and rich in K ions. The cell forms another protein, called Na pump that attaches to the luminal membrane of the cell. As soon as the Na reaches to the DCT from GFR, it is passed through this channel to the cell and finally to the extracellular fluid and then to the peritubular blood capillary. Along with Na, water is also reabsorbed. Na reabsorption increases the osmolarity of the blood and thus more water is reabsorbed and thus the venous blood volume increases. And if the venous blood volume is high meaning if high volume of blood reaches the heart, there would be more cardiac output.
(B) ADH – Anti Diuretic Hormone / Vasopressin
- This hormone is released from the posterior pituitary, but synthesized by the hypothalamus.
- This hormone is secreted when the blood osmolarity is high. This allows DCT and CT permeable to water. This makes concentrated urine. Once the osmolarity goes down from 300+, further secretion of ADH is stopped.
- The normal blood osmolarity is 300 mOs / L. if the osmolarity increases from 300 then only ADH will be secreted. 300 +osmolarity means, the solute concentration of the plasma fluid is more than the normal.
- Besides, there are certain osmoreceptors which are present in the hypothalamus that detects whether the osmolarity is high or lower than 300. Once the osmoreceptor detects high solute and less water, the thirst center in the hypothalamus is detected as a result, the person will feel thirsty and exogenous intake of water will take place.
(C) ANF (Atrial Natriuretic Factor):
- ANF is secreted by the wall of the atria.
- ANF is secreted in response to high blood pressure. High BP will cause higher concentration of Na in ECF, and high blood volume.
- ANF opposes RAAS and ADH
- This leads to Natriuresis meaning Na will pass out in the urine and dieresis (watery urine).
FORMATION OF URINE
Formation of urine takes place in different steps:
- Glomerular filtration
- Selective / tubular reabsorption
- Tubular secretion
GLOMERULAR FILTRATION
- It is a non-selective passive process because here what is being filtered is not screened rather they are screened only on the basis of size and not chemical properties. In this process blood plasma is filtered due to glomerular hydrostatic pressure (GHP).
- Glomerular filtration is under the effect of different pressure:
- Pressure favoring filtration is GHP. This pressure is developed due to the difference in the diameter of the afferent and efferent arteriole. In other words, from a broader afferent arteriole to a narrower efferent arteriole. GHP = 60 mm of Hg
- Pressure opposing filtration: 1. Blood colloidal osmotic pressure (BCOP): this pressure is developed due to colloids (proteins, mostly albumin) present in the blood. These albumins bind with water and do not allow moving out of the capillaries. BCOP = 30 mm Hg. Capsular Hydrostatic Pressure (CHP): this pressure develops due to fluids already present in the Bowman’s capsule. CHP = 20 mm Hg. In other words, some fluid is already present in Bowman’s space and more fluids are being filtered into the Bowman’s space. This creates an upward pressure by the already present fluid in the Bowman’s space in upward direction.
Effective / Net Filtration Pressure (EFP / NFP) = GHP – (BCOP + CHP)
= 60-(30+20)
= 10 mm of Hg
10 mm of Hg pressure is enough for the filtration of plasma. And the filtrate is called GLOMERULAR FILTRATE. This glomerular filtrate contains all the components present similar to the plasma except the proteins. Components of plasma include water, ions, glucose, amino acids, water soluble vitamins, urea, uric acid, antibiotics, etc.
GLOMERULAR FILTRATION RATE (GFR):
Normal GFR = 125 ml/min or 180 liters/day
There is autoregulation of GFR. If there is a disturbance leading to increase in GFR. The more filtrate in the renal tubule will be sensed by the macula densa as PCT will not be able to absorb solute due to fast filtration speed. As a result, less solute will be absorbed and macula densa will sense a high amount of Na, Cl and water in the renal tubule. This will trigger myogenic regulation in which afferent arteriole constricts to reduce the volume of blood coming for ultrafiltration. This results in less GFR. If this mechanism is not enough, another regulation starts called tubule glomerular regulation – this will inhibit NO (Nitric oxide – a vasodilator) and more constriction will occur in the afferent arteriole. The third regulation occurs through the sympathetic nervous system by releasing nor-epinephrine. It also cause constriction in the afferent arteriole to decrease GFR rate.
Renal Blood Flow: it is the amount of blood reaching the kidneys per unit time. Renal blood flow is 1100 to 1200 ml/min. Since only plasma is being filtered (renal plasma flow) so that would come around 600 – 700 ml/min.
Filtration fraction = ratio of GFR and RPF
= 600 / 125 or 700 / 125 = 16 – 20 %
Total blood = 5 liter
Plasma = 3 liter
Per day filtration = 180 / 3 = 60
It means, filtration is done 60 times in 24 hours.
Steps of Urine Formation
- Glomerular filtration
- Tubular reabsorption
- Tubular secretion
Tubular reabsorption:
Substances that are reabsorbed:
- High threshold substances – these substances are maximally reabsorbed. Example, water, glucose, amino acids, Na+, Cl-. Though these substances are maximally absorbed, but there is a threshold limit beyond which these substances could appear in the urine. The threshold up to which substances are reabsorbed from glomerular filtrate is called RENAL THRESHOLD. For instance, the renal threshold for glucose is 180 mg/ dL of blood.
- Low threshold substances – these substances are partially reabsorbed meaning some amount will be reabsorbed and some amount would appear in the urine. Example- urea, and uric acid,
- Non-threshold substances: these substances are not reabsorbed at all. In other words, the amount present in the blood plasma would appear in the glomerular filtrate and passed in the urine without any absorption. Example: creatinine, hippuric acid, and inulin, etc.
Tubular reabsorbtion in various parts of the nephron:
PCT: the walls of PCT is permeable to water and ions. So, in this region, water, Na+, Cl-, K+, HCO3-, glucose, vitamin C, amino acids, etc. are reabsorbed. Glucose, amino acids, and Na ions are reabsorbed actively, however, water and nitrogenous wastes are reabsorbed passively. The glomerular filtrate after absorption become isotonic to the blood plasma. 60% of the glomerular filtrate is reabsorbed. Example: water, Na, Cl, HCO3, glucose, vitamin C, amino acids, K ion, and a very little amount of urea and uric acid.
Descending Loop of Henle: wall of the descending limb is permeable to water only. So, in this region, water will move out of the descending limb to the interstitial space. As a result, the osmolarity of the filtrate becomes higher and higher as we go down the descending limb. In other words, we can say that the filtrate in the descending loop of Henle is HYPERTONIC. Example: water reabsorption
Ascending loop of Henle: it is only permeable for ions and not for water. So, the filtrate will release Na, Cl, Mg and Ca ions into the interstitial space. The transport of ions in the thin ascending loop of Henle is passive; however, the transport of ions in the thick ascending loop of Henle is through active process. As ions move out of the ascending loop of Henle, the concentration of the filtrate will decrease and the concentration will become HYPOTONIC. Example: Na, Cl, K, Mg, and Ca, etc.
DCT: when the filtrate reaches the DCT, it is hypotonic. The permeability of DCT is conditional – normally, DCT is not permeable to water, but in water stress condition, when ADH secretion starts in the blood. In that condition, the DCT becomes permeable to water. Na ion absorption is also conditional, which is under the effect of aldosterone. Example: water reabsorption under the effect of ADH hormone; Na ion reabsorption by the effect of aldosterone. Ca ion reasbsorption under the effect of PTH (Parathyroid hormone).
CD: The absorption is similar to DCT i.e., conditional for water and Na ion under the effect of aldosterone and ADH. When the filtrate reaches the CD, then we call it as URINE. Example: Conditional reabsortion of water, Na, Ca like the DCT. Urea is also reabsorbed in this region (in the medullary part).
Note: Under conditional reabsorption, the urine concentration would be HYPERTONIC.
Tubular Secretion: the peritubular capillary secreting some wastes to the renal tubule. Besides excretion, the kidneys perform various other functions such as balancing of ions, and maintenance of blood pH. So, the peritubular capillary releases H ions into the filtrate to maintain blood pH. The H ion is released in the PCT and some amount of (NH4+) ammonium ions, and K+ions as well. There is no secretion in the loop of Henle. In DCT, there is a secretion of H, K, and NH4 ions. Similarly, in CD, there is a secretion of H, K and NH4+ ions. Besides, little amount of creatinine and hippuric acids are also secreted.
Mechanism to concentrate the urine
The arrangement of nephron with the peritubular capillary is in such a way that maximum water could be taken out from the filtrate. This mechanism is called COUNTERCURRENT MECHANISM – -it is the arrangement of the loop of Henle and the peritubular capillaries in such a way that the glomerular filtrate and the blood flow in the opposite direction. This arrangement allows to concentrate the urine maximally by maintaining a high concentration of NaCl and urea in the medullary interstitium.
Structures involved in the countercurrent mechanism is the loop of Henle and Vasa recta (it is a peritubular capillary going along the side of the loop of Henle).
Note: the osmolarity of the cortical intetrstitium is 300 mOs/dl. However, the osmolarity of the medullar interstitium changes as we go downward in an increasing order up to 1200 mOs/dl.
The descending limb of vasa recta is associated with the ascending loop of Henle and the ascending limb of the vasa recta is associated with the descending loop of Henle. Now, in the medullary interstitium, the concentration of solute will increase because some urea will be secreted by the CD and from the ascending loop of Hencle Na and Cl ions will be secreted out by the renal tubule. As a result, due to high osmolarity of the medullary interstitium, maximum water will be reabsorbed from the glomerular filtrate along with the solute. However, if total solute would be reabsorbed, there would not be any elimination of the solute from the filtrate. Well, that’s where the countercurrent mechanisms works. When the descending vasa recta absorbs solutes and from the filtrate its solute concentration increases and when in the ascending vasa recta due to solute gradient, vasa recta will secrete salts from it and go to the medullary interstitium. That’s how the medullary interstitium concentration is maintained.
Note: vasa recta is fully permeable for salts, ions and water.
Individuals who take more protein are able to concentrate their urine efficiently because with more intake of protein, more urea will be formed and that will increase the solute concentrate of the medullary interstitium. Besides, animals who can concentrate their urine efficiently will have longer loop of Henle.
Urine is formed in the CD. Many CD will join together and form a common duct called the duct of Bellini. This common duct will open into minor calyx, then major calyx then renal pelvis to ureter and finally to the urinary bladder. From the bladder the urine will be passed out through the urethra.
Urine characteristics:
- Urine is a pale yellow color and this color is due to UROCHROME Urochrome is a byproduct of RBC’s breakdown.
- In a day, around 1 to 1.5 L of urine is produced
- 25-30 g of urea is removed per day
- pH = 6; pH varies from 4.2 to 8.2
- It is slightly heavier than water
- It contains 95% H2O
- The 5% includes urea, uric acid, K+, H+ NH4+, SO4, PO4, Oxalate, creatinine, hippuric acid
Abnormal constituent of Urine
- Glycosuria: glucose is present in urine. This occurs when a person is suffering from diabetes mellitus.
- Ketonuria: ketone bodies in the urine. This condition is also seen in diabetes mellitus. People with diabetes cannot metabolize glucose rather metabolize fat and ketone bodies are produced out of it. Besides, ketone bodies are also seen during starvation because in that case body fat will start to break.
- Albuminoria: Albumins are present in the urine. This occurs due to the inflammation in the glomerulus. As a result, albumins pass through the glomerular capillaries to the filtrate.
- Haematuria: blood in the urine. This occurs due to kidney stone and when the stone (renal calculi) passes through the ureter due to friction it damages the wall.
- Haemaglobinuria: heamoglobin in the urine. This condition occurs due to the rupturing of RBC (haemolysis).
- Pyuria: pus cells in the urine. It occurs due to infection because push is nothing but dead WBC (neutrophils).
- Xanthinuria: Xanthine in urine. Xanthine is an intermediate formed during purine metabolism. We know the purine breaks up to form uric acid but there is an intermediate compound formed, called Xanthine and to form uric acid from xanthine, xanthine oxidase enzyme is required. If that enzyme is lacking then xanthine would appear in the urine. This is thus a genetic disorder. Xanthine can also form crystals to form stones called xanthine calculi.
MICTURITION
Voiding of urine from the urinary bladder.
In the urinary bladder, there are two sphincters – the internal sphincter is involuntary and the external sphincter is voluntary. These sphincters are connected through the nervous system. The nerve connected to the external sphincter is PUDENDAL NERVE. Stretch receptor nerves are connected to the urinary bladder. There is a supply of sympathetic and parasympathetic nervous contact to the urinary bladder. The sympathetic nervous system keep the urinary bladder in relaxed state during the filling of bladder. And the sphincters would be constricted when the bladder is in relaxed state.
After filling of the urinary bladder, it is stretched as a result, the stretch receptors are stimulated. This sends a message to the brain. The pudendal nerve is inhibited; sympathetic nervous system is inhibited and parasympathetic nervous system is activated. Now the bladder contracts and the internal sphincter relaxes and the urine passes out of the urethra.
Apart from the kidneynes, there are accessory excretory organs present.
Accessory Excretory Structures
Liver: When some toxins are taken through the food, before it enters the blood, it reaches the liver through the hepatic portal system. In liver, the toxin is detoxified. Besides, liver is also concerned with the synthesis of urea.
Lungs: Remove CO2 and some amount of water vapor. Nearly 18 liters of CO2 are removed per day.
Sweat: the primary function of sweating is to regulate the body temperature. Sweat contains water and a little amount of urea, lactic acid, etc.
Sebum: the secretion from the oil glands. This secretion contains hydrocarbons, waxes, steroids, etc.
Some of the Disorders of the Kidney of the Human Excretory System
Each kidney has 1 million nephrons. These nephrons are constant in number and new nephrons are not formed after birth.
Cystitis: inflammation of urinary bladder.
Pyelonephritis: inflammation of renal pelvis.
Glomerulonephritis: inflammation of the nephron.
Uraimia: high blood urea. It causes toxicity of the body tissues. The person feel lethargic and does not feel like eating – the condition called anorexia.
The excess urea can be removed artificially through haemodialysis or the artificial kidney.
Process of Hemodialysis

Steps of hemodialysis:
- The blood is taken out through the radial artery (present on the radius of the hand) through a catheter. This blood is passed through a cool chamber (O degree Celsius); heparin is mixed in blood to avoid coagulation. This blood is passed through a system of tubes (spiral tube), which are kept in a chamber containing a dializing fluid. These tubes are formed of cellophane (permeable). The dializing fluid has the same constituent as the blood plasma, only it is devoid of waste materials such as urea and uric acid.
- The wastes in the spiral tube comes out into the dializing fluid and this will occur until the isosmotic condition is reached.
- In order to remove wastes from the blood, fresh dializing fluid is put into the chamber and the used one is taken out on a constant basis.
- After that the purified blood is returned to the radial vein after raising the blood temperature to 37 degree Celsius.
Kidney Transplant: matching donor is needed for this purpose. Only in case of identical twins, there is no problem in transplant; however, in case of a donor, CYCLOSPORIN, an immunosuppressant is given to the recipient. It is obtained from the fungus.